Patient volume is tumbling due to elective surgery and travel restrictions, “shelter in place” recommendations, state-mandated closures, and patients' greater reluctance to visit emergency departments.
Since the COVID-19 crisis started, patient volume has fallen by an average of 60 percent for medical practices (nearly 75 percent of the over 700 organizations surveyed by the Medical Group Management Association last April were independent medical practices with fewer than 50 full-time equivalent physicians).
Emergency rooms have reported dramatic drops in even those visits that are especially critical and could depend on someone living or dying. Stanford University Medical Center, for example, which usually has 12 to 15 patients in their inpatient stroke unit, had none during one day in April – this was a first.
A review of insurance claims filed between March 1 and April 30 of this year demonstrated a 40 percent decrease in emergency department visits and a 47 percent decline in observation visits (which are commonly used for the evaluation of chest pain). The same study revealed a 93 percent drop-off in lab tests ordered from the emergency department and a 78 percent decline in tests ordered in urgent care centers.
Despite recent direct-to-consumer pleading from hospitals urging patients receive face-to-face care when needed for emergent conditions, patients are hesitant to receive face-to-face care. Similarly, data from the United Kingdom reveals a 50 percent decline in emergency room visits for chest pain in recent weeks. In the meantime, in the US, consider that an estimated 85 patients are dying in their homes from heart attacks every day.
Not All Care Can Be Remote Care
Essential healthcare wasn't prohibited before the crisis began. Just walking into a clinic or emergency room wasn't something people once thought could put their health further at risk. There's thus been great confusion among consumers about what “essential medical care” really is during these times. And what to do if they need to see someone face-to-face, like have surgery.
As hospitals and health systems commence opening procedures, the measures they are taking to ensure patient and staff safety are resulting in a necessary reconceiving of the fundamental manner in which care is delivered. For example, alternate access points are being constructed to segregate COVID-19 and accommodate social distancing guidelines. Patient scheduling is being upended in real-time in every area of the enterprise to enable social distancing. These measures will result in less office throughput of patients, protracted procedural area turn-over, and the necessity to extend areas of operation into evenings and weekends to meet pent up demand.
For outpatient surgery and other interventional procedures, additional steps to protect both patients and staff from the aerosols generated during routine activities such as induction of anesthesia or the performance of the upper gastrointestinal tract endoscopy will be needed. Patients with any active respiratory conditions will receive telephonic screening 7 days and 24 hours before the procedure. If febrile or demonstrating symptoms of any kind, they will be rescheduled. We anticipate high cancellation rates as physicians err on the side of safety while we continue to refine our methods of diagnosing and treating COVID-19. Systematic screening for COVID-19 antigen or ribonucleic acid will be performed either the night before the procedure or done immediately before the procedure using a rapid test. We expect an increase in remote preoperative assessment and postoperative care. Everyone will wear masks – including patients, visitors (restricted by numbers and time in the facility), and staff. Special precautions will be used for higher-risk procedures, if these procedures are done at all. This is all merely a start.
The combination of a universal lack of antibody to COVID-19 and the current unavailability of an effective vaccine, and ongoing community circulation, means that occasional local or regional outbreaks can be anticipated and planned for. For the next two years or more, the elderly, infants, young vulnerable children, and high-risk individuals such as asthmatics and the immunocompromised may need to “shelter in place” while the general population continues social distancing efforts. Because these individuals are most in need of specialty medical care because of their burden of chronic disease and frailty, they will likely need to curtail in-person visits to physicians.
For the Next 24 Months, Telehealth for Many is the Safest Means of Receiving Medical Care
Within weeks of the outbreak onset in the US providers like American Well reported dramatic increases in consumer use of their services with volume increases ranging from 50 percent to 1,000 percent, according to Becker’s Hospital Review. Provider systems with prior established telehealth services saw 10- to 20-fold increases in usage by both patients and providers.
The current epidemic and the associated changes in reimbursement of telehealth services have resulted in an explosion of telehealth use by physicians, ancillary health services, and patients.
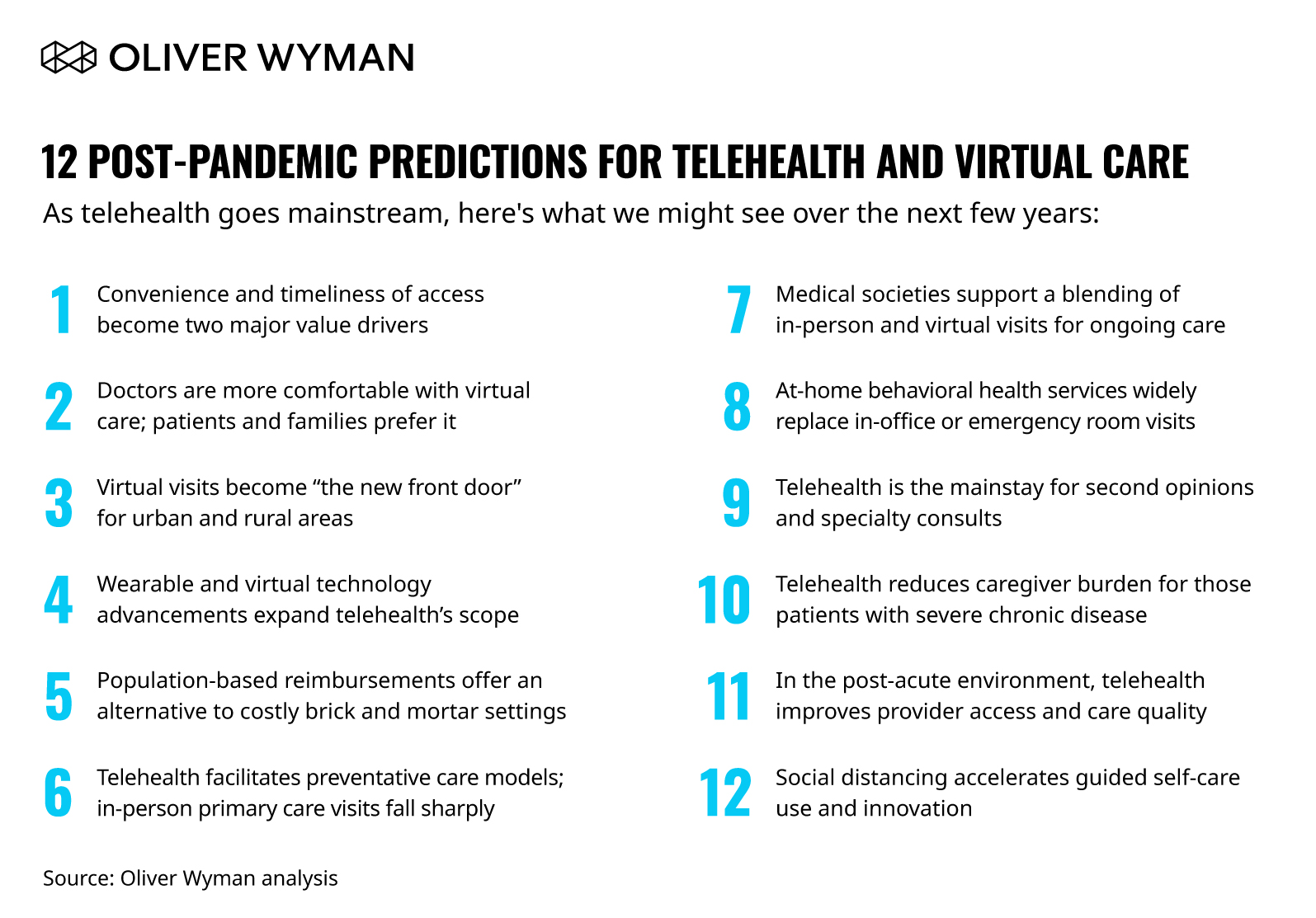
As we look to the future, here’s what we expect may unfold in time:




402x402.jpg.imgix.threeColumnTile.jpg)
